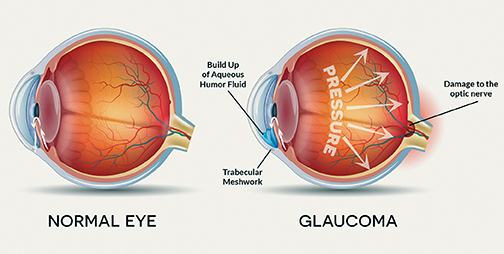
Glaucoma is a condition that causes damage to your eye’s optic nerve and is one of the leading causes of blindness in the United States, affecting more than 3 million people. It can occur at any age but is more common in older adults.
The most common form of glaucoma has few symptoms or warning signs. It’s often linked to a buildup of pressure inside your eye. The increased pressure, called intraocular pressure, can damage the optic nerve, which transmits images to your brain. The effect is so gradual that you may not notice a change in vision until the condition is at an advanced stage.
It’s important to have regular eye exams that include measurements of your eye pressure. People who are over 40 should have a dilated eye examination from an ophthalmologist or optometrist at least every two years. Those who are over 35 and have a family history of glaucoma; and everyone age 60 or older should schedule a comprehensive eye examination every year.
If you have the condition, you’ll generally need treatment for the rest of your life. Glaucoma can be treated with eye drops, pills, laser surgery, traditional surgery or a combination of these methods. The goal of any treatment is to prevent loss of vision, as vision loss from glaucoma is irreversible. The good news is that glaucoma can be managed if detected early, and that with medical and/or surgical treatment, most people with glaucoma will not lose their sight.
According to the Glaucoma Research Foundation (glaucoma.org) there are five common tests used to detect glaucoma:
Tonometry
Tonometry measures the pressure within your eye. During tonometry, eye drops are used to numb the eye. Then a doctor or technician uses a device called a tonometer to measure the inner pressure of the eye. A small amount of pressure is applied to the eye by a tiny device or by a warm puff of air.
The range for normal pressure is 12-22 mm Hg (“mm Hg” refers to millimeters of mercury, a scale used to record eye pressure). Most glaucoma cases are diagnosed with pressure exceeding 20mm Hg. However, some people can have glaucoma at pressures between 12 -22mm Hg. Eye pressure is unique to each person.
Ophthalmoscopy
This diagnostic procedure helps the doctor examine your optic nerve for glaucoma damage. Eye drops are used to dilate the pupil so that the doctor can see through your eye to examine the shape and color of the optic nerve.
The doctor will then use a small device with a light on the end to light and magnify the optic nerve. If your intraocular pressure is not within the normal range or if the optic nerve looks unusual, your doctor may ask you to have one or two more glaucoma exams: perimetry and gonioscopy.
Perimetry
Perimetry is a visual field test that produces a map of your complete field of vision. This test will help a doctor determine whether your vision has been affected by glaucoma. During this test, you will be asked to look straight ahead and then indicate when a moving light passes your peripheral (or side) vision. This helps draw a “map” of your vision.
Do not be concerned if there is a delay in seeing the light as it moves in or around your blind spot. This is perfectly normal and does not necessarily mean that your field of vision is damaged. Try to relax and respond as accurately as possible during the test.
Your doctor may want you to repeat the test to see if the results are the same the next time you take it. After glaucoma has been diagnosed, visual field tests are usually done one to two times a year to check for any changes in your vision.
Gonioscopy
This diagnostic exam helps determine whether the angle where the iris meets the cornea is open and wide or narrow and closed. During the exam, eye drops are used to numb the eye. A hand-held contact lens is gently placed on the eye. This contact lens has a mirror that shows the doctor if the angle between the iris and cornea is closed and blocked (a possible sign of angle-closure or acute glaucoma) or wide and open (a possible sign of open-angle, chronic glaucoma).
Pachymetry
Pachymetry is a simple, painless test to measure the thickness of your cornea – the clear window at the front of the eye. A probe called a pachymeter is gently placed on the front of the eye (the cornea) to measure its thickness. Pachymetry can help your diagnosis, because corneal thickness has the potential to influence eye pressure readings. With this measurement, your doctor can better understand your IOP reading and develop a treatment plan that is right for you. The procedure takes only about a minute to measure both eyes.
Diagnosing glaucoma is not always easy, and careful evaluation of the optic nerve continues to be essential to diagnosis and treatment. The most critical concern is protecting your sight. Doctors look at many factors before making decisions about your treatment. If your condition is particularly difficult to diagnose or treat, you may be referred to a glaucoma specialist. A second opinion is always wise if you or your doctor become concerned about your diagnosis or your progress.